Beyond Medicine: Unmasking Pitt & America's Healthcare Crisis
Editor's Note: A deeper look into the challenges facing the University of Pittsburgh Medical Center (UPMC) and their reflection of broader systemic issues within the American healthcare system has been published today.
Why This Matters: The struggles faced by UPMC, a prominent healthcare system, aren't isolated incidents. This article explores the complex interplay of factors contributing to America's healthcare crisis, using UPMC as a microcosm to illuminate broader systemic issues impacting access, affordability, and quality of care. Keywords like healthcare affordability, healthcare access, hospital pricing, physician shortages, and patient advocacy are explored in detail.
Key Takeaways of Pitt & America's Healthcare Crisis:
| Takeaway | Description |
|---|---|
| Rising Healthcare Costs | Examines the escalating expenses associated with healthcare in the US and their impact on individuals and the economy. |
| Limited Healthcare Access | Explores the barriers preventing many Americans from accessing necessary medical care. |
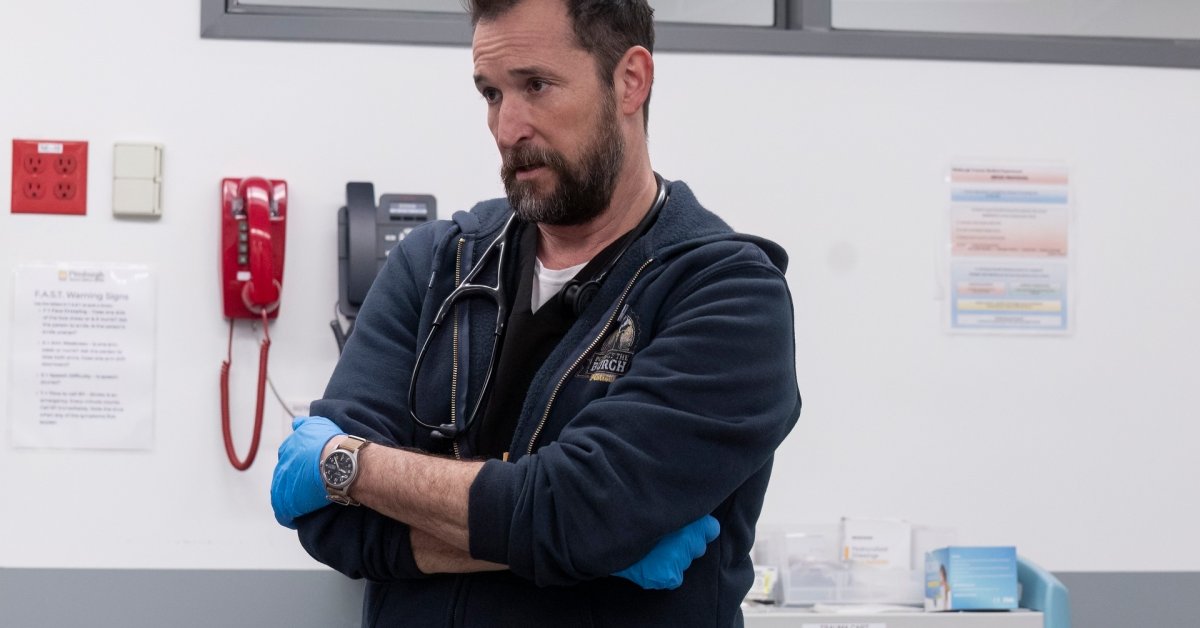
| Physician Shortages and Burnout | Discusses the critical shortage of healthcare professionals and the associated burnout rates. |
| The Role of Large Hospital Systems | Analyzes the influence and impact of large hospital systems like UPMC on healthcare delivery and costs. |
| Advocacy and Policy Solutions | Investigates the role of patient advocacy and necessary policy changes to improve the system. |
Beyond Medicine: The Pitt & America's Crisis
Introduction: The University of Pittsburgh Medical Center (UPMC) stands as a prominent player in the American healthcare landscape. However, its challenges serve as a stark reminder of the broader, systemic issues plaguing the nation's healthcare system. This article explores these interconnected problems, examining how UPMC's experiences reflect the larger crisis.
Key Aspects of the American Healthcare Crisis
- High Costs: The escalating cost of healthcare is a major factor contributing to the crisis. This impacts patients' ability to afford care, insurance premiums, and overall economic strain.
- Limited Access: Geographical limitations, lack of insurance, and bureaucratic hurdles restrict many Americans from accessing quality healthcare.
- Physician Shortages: A significant shortage of doctors and nurses, coupled with increasing burnout rates among healthcare professionals, further exacerbates the problem.
- Hospital Consolidation: The increasing consolidation of hospital systems, exemplified by UPMC's size and influence, can lead to concerns regarding market dominance and pricing strategies.
- Lack of Transparency: Limited transparency in hospital pricing and billing practices makes it difficult for patients to understand and navigate healthcare costs.
UPMC: A Case Study
Introduction: UPMC's position as a major healthcare provider allows for a detailed examination of the challenges impacting the entire sector.
Facets of UPMC's Challenges:
- Role: UPMC plays a significant role in providing healthcare in Pennsylvania and beyond, yet faces similar pressures as other large healthcare systems.
- Examples: Specific instances of high costs, limited access, and potential issues concerning transparency can be analyzed within the UPMC context.
- Risks: The risks associated with market consolidation and potential negative impacts on patient care need to be considered.
- Mitigation: Possible mitigation strategies that UPMC and other systems can employ to address these challenges are examined.
- Impacts: The impact of UPMC's challenges on patients, the local community, and the broader healthcare system is assessed.
- Summary: The analysis of UPMC highlights the systemic nature of the challenges within the American healthcare system.
The Interplay of Physician Shortages and Healthcare Costs
Introduction: Physician shortages directly contribute to increased healthcare costs through reduced access to care, longer wait times, and potential reliance on more expensive emergency services.
Further Analysis: The article will explore how reduced physician availability contributes to delayed diagnoses, higher treatment costs due to worsening conditions, and overall strain on the healthcare infrastructure.
Closing: Addressing physician shortages requires multifaceted approaches including increased medical school enrollment, improved working conditions to reduce burnout, and incentivizing primary care practices. This is directly linked to reducing healthcare costs and improving overall access.
Key Insights into the Crisis (Information Table)
| Factor | Impact | Potential Solutions |
|---|---|---|
| High Costs | Reduced access, financial strain, economic burden. | Price transparency, regulatory reform, cost-containment measures. |
| Limited Access | Delayed or forgone care, worsening health outcomes. | Expanding insurance coverage, improving rural healthcare access. |
| Physician Shortages | Longer wait times, increased emergency room usage, reduced quality of care. | Increasing medical school enrollment, improving working conditions. |
| Hospital Consolidation | Potential market dominance, increased prices. | Antitrust regulations, promoting competition. |
FAQ
Introduction: This section addresses common questions and misconceptions surrounding the American healthcare crisis.
Questions:
- Q: Why are healthcare costs so high in the US? A: A combination of factors including high administrative costs, expensive pharmaceuticals, and the fee-for-service model contribute to high costs.
- Q: What can I do to advocate for healthcare reform? A: Contact your elected officials, support patient advocacy groups, and educate yourself on healthcare policy.
- Q: Is there a solution to the physician shortage? A: Addressing physician shortages requires a multi-pronged approach including increasing medical school enrollment, improving working conditions, and incentivizing primary care.
- Q: How does UPMC's situation reflect the national problem? A: UPMC's challenges, like high costs and access issues, mirror similar challenges faced by other large healthcare systems across the nation.
- Q: What role does insurance play in the crisis? A: The current insurance system, while providing coverage for many, still leaves significant gaps in access and affordability for millions of Americans.
- Q: What is the long-term outlook for the American healthcare system? A: The future of the system depends on addressing the systemic issues outlined above through policy changes and systemic reform.
Summary: The FAQ section highlighted the complexity of the American healthcare crisis and the need for comprehensive solutions.
Tips for Navigating the Healthcare System
Introduction: These tips can help individuals better navigate the complexities of the American healthcare system.
Tips:
- Understand your insurance coverage thoroughly.
- Shop around for healthcare services to compare prices.
- Utilize preventive care to reduce long-term healthcare costs.
- Ask questions and advocate for yourself with healthcare providers.
- Be aware of your rights as a patient.
- Consider joining a patient advocacy group.
- Utilize telehealth options for convenient and often more affordable care.
- Be proactive in managing your health to reduce the need for expensive interventions.
Summary: Proactive engagement and informed decision-making can empower individuals to better manage their healthcare experiences.
Resumen de la Crisis de Atención Médica en Estados Unidos (Summary of the US Healthcare Crisis)
Summary: This article explored the multifaceted challenges facing the American healthcare system, using UPMC as a case study. The high cost of care, limited access, physician shortages, and the impact of hospital consolidation were all discussed, highlighting the urgent need for comprehensive reform.
Mensaje Final (Closing Message): The future of healthcare in America hinges on collaborative efforts to address systemic issues. Through policy changes, increased transparency, and a renewed focus on patient well-being, we can work towards a more equitable and affordable healthcare system for all. Let's advocate for change and demand a healthier future.